PulseCam peeks below skin to map blood flow
HOUSTON – (April 13, 2020) – Rice University engineers have found a way to use a video camera to peek below the skin and make high-resolution maps that show doctors and nurses exactly how much blood is reaching the capillaries.
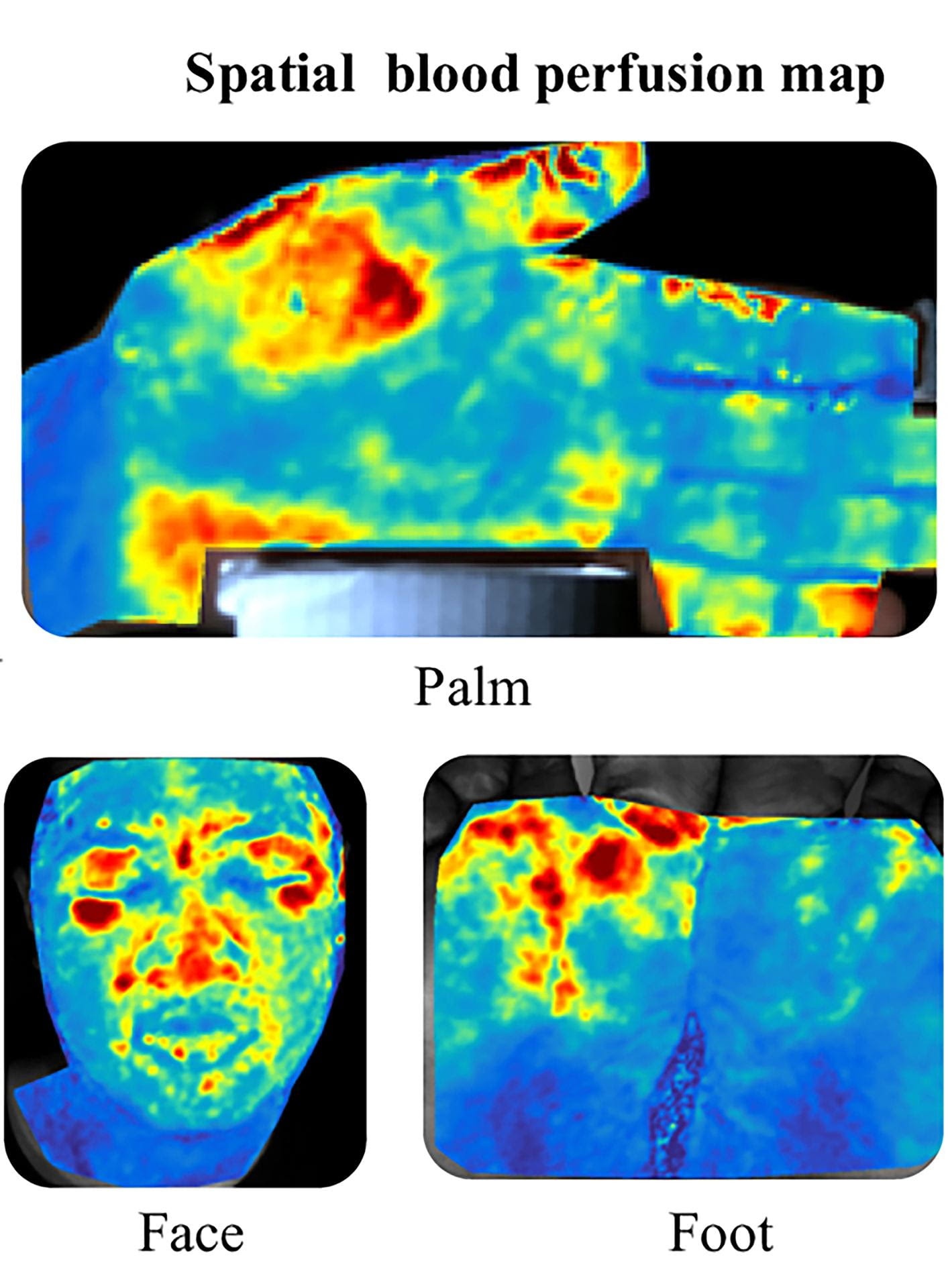
PulseCam uses a patented process to combine information from video recordings and a pulse oximeter to create high-resolution blood perfusion maps.
Blood flows from the heart in waves, and anyone who’s taken a pulse by hand has felt the crests of those waves. Pulse oximeters measure the crests, troughs and duration to produce a “pulse waveform,” the zigzag readout that’s often displayed on bedside monitors in hospitals.
“PulseCam uses a camera feed to calculate the strength of that waveform at hundreds of points on the surface of the skin,” said Ashutosh Sabharwal, a professor and chair of the Department of Electrical and Computer Engineering (ECE) in Rice’s Brown School of Engineering.
In a recent paper in the peer-reviewed journal Scientific Reports, Sabharwal and ECE’s Ashok Veeraraghavan, Baylor College of Medicine surgeon James Suliburk and former Rice Ph.D. student Mayank Kumar demonstrated the technology in several clinically relevant settings.
In one study, PulseCam was used to monitor blood perfusion in the palms of 10 surgical patients as they were undergoing general anesthesia.
“With this technology we can measure perfusion in a new way never done before, giving us new insight into disease process,” Suliburk said.
Sabharwal said blood vessels dilate when anesthesia is administered.
“They essentially become bigger pipes, very suddenly, and perfusion increases dramatically,” he said. “Then, as the anesthesia sets in, perfusion gradually decreases as the body finds a new stable point.”
In the images from the surgeries, PulseCam clearly shows the rapid influx of blood from dilation of vessels at the site of the two major arteries that supply blood to the hand.
“The main challenge for us is that no other device can noninvasively measure blood flow with this level of detail,” Sabharwal said. “Since we can’t measure against a proven method, we can’t make claims about the correctness of our measurements.”
That’s why the team developed innovative methods to establish a range of clinically relevant demonstrations, he said.
“We’re in a unique situation where we have to find ways to bring about predictable changes in blood flow — like dilation from anesthesia or the restriction of flow, which is called vascular occlusion — and show our measurements match the outcomes that we expected based on human physiology.”
In another of the paper’s demonstrations, Kumar used PulseCam to record blood perfusion in the hands of Rice graduate students during a standard noninvasive diagnostic test that uses an inflatable pressure cuff like those used to measure blood pressure. In the tests, the students’ upper arms were squeezed tightly for a few seconds to restrict blood flow to the hand. Then the pressure was released, and blood flow returned.
It takes PulseCam about 30 seconds to deliver a high-resolution blood perfusion map, and it can update the map every 10 seconds, Sabharwal said. It generates the maps based on slight color changes caused by perfusion.
Because of the time needed to resolve an image, PulseCam works only if a subject is relatively still. It also delivers unprecedented resolution. In the diagnostic demonstration with students’ hands, for example, the researchers showed PulseCam could distinguish the difference between a blocked artery and a blocked vein. Arterial and venous occlusion are each clinically important, but physicians have no direct way to measure venous occlusion.
“We can actually sense small changes in pressure, which is very important, from a clinical point of view,” Sabharwal said. “Knowing there’s reduced blood flow is important, but if we can tell whether it’s 10% lower or 30% lower, that’s useful clinical information. This could help improve the quality of care for patients with deep vein thrombosis, for example.”
Sabharwal and Suliburk, an associate professor of surgery at Baylor, said PulseCam shows what’s possible when engineers and clinicians work closely together.
“As clinicians, we’re focused on continuously improving patient care,” Suliburk said. “New technologies can help, and this project shows the magnitude of innovation that is possible when clinical experts in the Texas Medical Center work hand in hand with engineering experts at Rice.”
Veeraraghavan is an associate professor of electrical and computer engineering at Rice.
The research was funded by the National Science Foundation.





